Stem cell treatment for osteoporosis, a form of regeneration therapy, stands out as one of the most promising ways to treat degenerative bone conditions.
Regencord has established itself as a global leader in stem cell therapy. The center’s records reveal many cases where bone stem cells helped osteoporosis patients build new bone tissue. One patient case highlights the treatment’s broader benefits. He saw major improvements in his joint pain and overall health markers after the therapy.
This piece explores the science of stem cell treatment for osteoporosis. You’ll learn how bone regeneration works and examine the evidence showing its impact on bone density and quality of life.


Osteoporosis breaks down bone structure significantly, but patients don’t notice any warning signs until the damage becomes severe. Known as the “silent disease,” osteoporosis happens when bones break down faster than they can rebuild, making them weak and likely to break. This condition affects about 10 million men and women in the United States alone.
Many people think osteoporosis only affects older white women, but the condition can affect men and women of all races. The disease speeds up after age 50, and both men and women lose 1-3% of their bone mass each year without medical treatment.
Bone density slowly decreases as the internal framework breaks down during the silent phase. This breakdown continues without any signs, making it hard to catch early. People’s bones are strongest in their early 30s, and after that, bone loss starts to happen faster than new bone formation. Women lose bone much faster after menopause because their estrogen levels drop.
Most people discover they have osteoporosis after an unexpected break from a minor injury - like breaking a bone from a small fall, coughing, or just bending over. Other warning signs include:
Bone density scans (DXA) are the main tool doctors use to check if someone has or might get osteoporosis.
Osteoporosis shows up as pain, broken bones, and physical problems that end up causing a loss of independence and a need for long-term care. The pain comes from both tissue damage and nerve problems.
Vertebral compression fractures cause most osteoporosis pain. But chronic pain can last long after breaks heal for several reasons. Weak bones lead to multiple fractures over time, which change posture and force back muscles to stay tight. This creates muscle tiredness and ongoing pain.
Research shows clear connections between chronic low back pain and osteoporosis, especially in older people. So, osteoporosis-related fractures reduce the quality of life in physical, mental, and social ways.
Research shows that osteoporosis patients score lower in physical and social activities compared to people with normal bone density. It also shows that patients with past osteoporotic fractures have a lower health-related quality of life than those without breaks.
Despite treatment guidelines, managing osteoporosis remains difficult. Standard treatments mostly involve medications and lifestyle changes. Bisphosphonates, denosumab, and parathyroid hormone can cut fracture risk in half. However, these treatments have major limitations.
Most current treatments try to slow bone loss rather than rebuild damaged bone. Bisphosphonates block bone breakdown cells, while denosumab reduces how many of these cells form. But medications often don't help enough with pain.
Standard medications can also cause rare but serious side effects, including unusual thigh bone breaks and jawbone problems. Many patients with osteoporosis get no treatment even after diagnosis - about 25% of Australian patients with diagnosed osteoporosis never received medications.
Mixing primary and secondary prevention in osteoporosis treatment makes management more complex. Standard treatments also don't address quality-of-life issues, and most rehabilitation programs don't properly track improvements in pain or physical function.
These limits have created interest in new approaches, including whether stem cells might help osteoporosis by rebuilding bone tissue instead of just slowing its breakdown. The possibility that stem cells could repair bones represents a big transformation from traditional treatment approaches.
Bone tissue can regenerate itself remarkably well. This power decreases with age and conditions like osteoporosis. Stem cell therapy uses the body’s natural healing mechanisms to reverse osteoporotic changes rather than just slow down the deterioration. The way these cells work creates the foundation to appreciate their therapeutic potential.
Stem cells stand out because of two unique features: they can make copies of themselves through cell division (self-renewal) and turn into different specialized cell types (differentiation). Unlike cells with specific jobs, stem cells stay undifferentiated until their environment signals them to become repair cells.
The environment around stem cells plays a vital part in guiding their behavior. These cells respond to local factors at injury sites and develop into specific cell types needed for healing—bone, cartilage, muscle, or ligament. This responsiveness to their surroundings makes them perfect candidates for regenerative medicine.
Healthy people's stem cells constantly help maintain and repair tissue. This regenerative power can weaken depending on the size of tissue damage or certain diseases. Age and osteoporosis cause bone-forming stem cells to decline in number and function, leading to reduced bone formation.
Scientists study various kinds of stem cells to treat osteoporosis. Each type has its source, ability to change into different cells, and practical uses:
Bone regeneration balances old bone breakdown with new bone formation while creating blood supply to these areas. Stem cells influence this process in multiple ways.
Local skeletal stem cells start the fracture healing process with little help from circulating stem cells. Removing these cells disrupts bone regeneration and remodeling, which shows how important they are. MSCs help build bone directly by becoming osteoblasts and indirectly through their secretions.
MSCs release bioactive molecules like growth factors and cytokines that control bone formation. These include insulin-like growth factor (IGF-1), transforming growth factor (TGF-β), and vascular endothelial growth factor (VEGF). Together, these factors boost osteoblast activity and help form blood vessels needed for healthy bone.
New research shows that MSCs can reduce inflammation and modify immune responses. They decrease inflammatory responses after acute injury and suppress immune cells that might contribute to bone loss. This comprehensive approach explains why stem cell treatment shows more promise than traditional therapies that target only one aspect of bone metabolism.
Scientists now study extracellular vesicles (EVs) from stem cells. These tiny particles carry proteins, lipids, and genetic material that can send bone-promoting signals without needing whole-cell transplants. This cell-free method avoids many complications of traditional stem cell therapy while offering similar benefits.
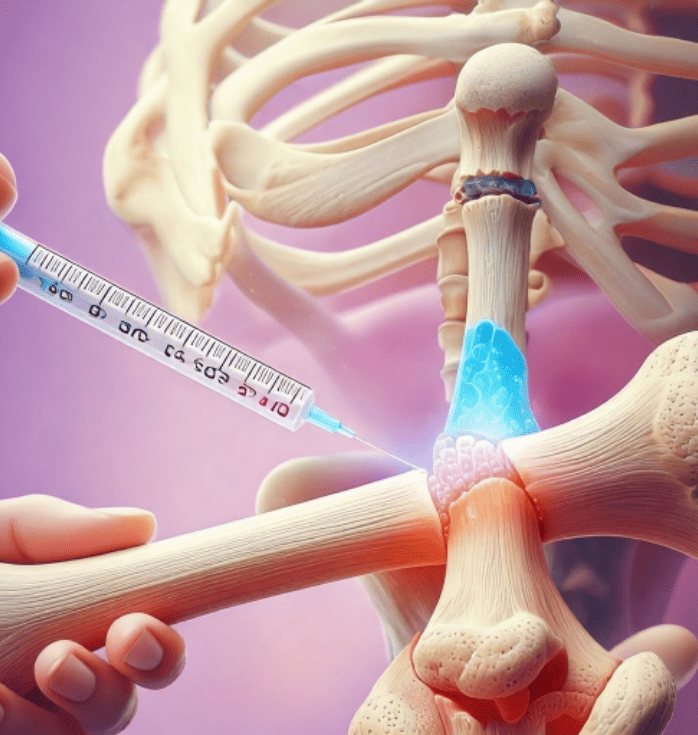

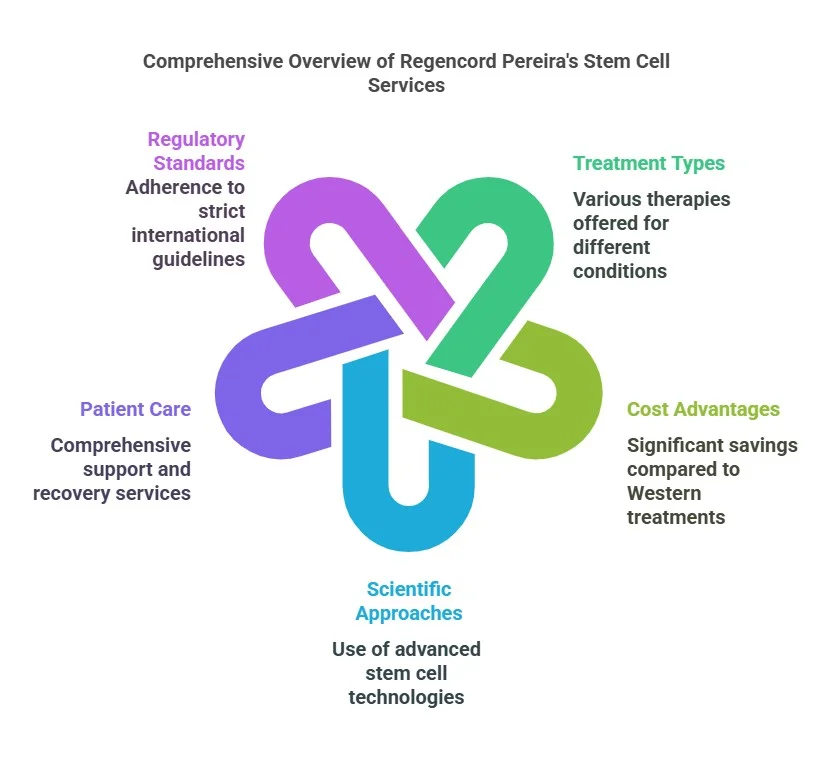
Regencord’s stem cell treatment for osteoporosis represents a fundamental change from traditional treatments that only slow down bone loss. This therapy tackles the root cause of bone remodeling imbalance. It promotes regeneration instead of just preventing further deterioration.
Regencord’s protocol uses mesenchymal stem cells (MSCs) from bone marrow, adipose tissue, or the umbilical cord. These sources give cells that can effectively build new bone tissue. The treatment team harvests, processes, and delivers concentrated doses of MSCs to jumpstart bone renewal. These cells know how to find injured areas by following specific signals and repairing damaged tissue. Stem cell homing, the process by which these cells navigate to the target site, is crucial for the treatment’s success.
Boosting osteoblast function sits at the heart of osteoporosis treatment. Patients with osteoporosis have fewer MSCs that can become osteoblasts, and these cells don't work as well as they should. This results in less bone formation. The MSCs we introduce during treatment help fix bone formation through:
These mechanisms work together to increase osteoid secretion, which builds new bone tissue.
Regencord's treatment actively controls excessive osteoclast activity. Clinical studies show that MSCs block osteoclast development and function through the PI3K/Akt/NF-κB signaling pathway. This helps restore balance to the osteoblast-osteoclast relationship that osteoporosis disrupts. The treatment reduces both the number and size of multinucleated osteoclasts, which slows down bone loss.
Regencord's approach's healing power goes beyond direct cellular effects. MSCs act as "medicinal signaling cells" and release bioactive molecules, including IGF-1, TGF-β, VEGF, angiogenin, and hepatocyte growth factor. These substances help create new blood vessels that keep bones healthy.
MSCs also have powerful immune-balancing properties that lower inflammation, which is linked to osteoporosis getting worse. This matters because inflammatory factors often trigger too much osteoclast activity and destroy bone. Clinical applications show that MSCs help mostly by creating a healing environment rather than just turning into bone cells.
Regencord's stem cell treatment offers a complete solution to osteoporosis by targeting multiple aspects of bone metabolism at once. Traditional treatments don't deal very well with this complex approach.
Scientific evidence shows stem cell therapy could help treat osteoporosis. This breakthrough has moved beyond theory and shows measurable benefits in labs and clinics.
Animal studies consistently show promising results. A meta-analysis of controlled studies revealed that genetically modified stem cell transplantation substantially improved bone mineral density (BMD) and bone volume/total volume (BV/TV) in osteoporotic animal models. MSC treatments showed increased bone mineral density and better osteogenic differentiation in rats, mice, rabbits, and goats.
The way doctors administer treatment makes a difference. Scientists have tested various delivery methods, such as tail vein injection, local injectable fillers, and intraperitoneal injection. Mouse models with age-related osteoporosis showed remarkable results—a single intravenous MSC injection doubled bone renewal rates and restored healthy bone architecture.
Clinical evidence looks promising even though research continues. MSC transplantation has led to substantial improvements in several bone-related markers. Studies confirm increases in trabecular number (Tb.N), trabecular thickness (Tb.Th), and cortical thickness (Ct.Th) while trabecular spacing (Tb.Sp) decreased.
The benefits go beyond structural changes. Stem cell therapy improves physiological markers of bone health. Treated patients show higher serum levels of calcium, alkaline phosphatase, and osteocalcin—all signs of active bone formation.
Real-life outcomes match these research findings. A 54-year-old patient's condition improved from osteoporosis to osteopenia after treatment in 2008. Another patient said, "I have actually reversed my osteoporosis to osteopenia," with a remarkable 5.4% increase in bone density.
Patient stories reveal quality-of-life improvements beyond numbers. Three out of four women in an early clinical trial reported less pain after MSC treatment. None of them experienced new osteoporosis-related fractures during follow-up.
Large-scale human trials remain limited. Yet, evidence from lab studies, animal research, and original human treatments suggests stem cell therapy offers hope - especially for patients who don't respond well to standard treatments.


Traditional osteoporosis medications don’t work well enough, even though doctors prescribe them widely. Stem cell treatment represents a transformation in how we treat this condition.
Standard osteoporosis drugs are used mostly to prevent bone loss instead of rebuilding damaged tissue. Bisphosphonates remain the go-to treatment but come with significant risks when used long-term. Patients might experience atypical femoral fractures, osteonecrosis of the jaw, and digestive system problems.
The numbers tell a concerning story. All but one of these commercially insured patients who break their hips receive osteoporosis medication within six months. Treatment rates have dropped significantly from 15% to 8% in the last decade. The situation becomes more alarming as 20-30% of people don’t survive beyond a year after a hip fracture.
Other medications bring their own set of problems. Denosumab can trigger bone loss when stopped. Hormone replacement therapy increases the chances of stroke, venous thromboembolism, and breast cancer.
Stem cell therapy surpasses the symptom-management approach by targeting why it happens. MSCs can adjust bone remodeling through multiple mechanisms, unlike drugs that just slow down deterioration. These cells create supportive regenerative environments through paracrine effects, which gives them a revolutionary advantage.
Stem cells' immunomodulatory properties are a great way to get better results, as they reduce inflammation linked to bone loss. This integrated approach means one treatment tackles several osteoporosis pathways simultaneously.
Regenerative approaches offer lasting benefits that regular treatments can't match. Stem cell therapy might lower osteoporotic fracture risk by actually restoring bone, not just slowing its breakdown. This is particularly important for preventing fragility fractures, which are a major concern for osteoporosis patients.
Recent studies show that stem cell-derived extracellular vesicles provide similar benefits without needing complete cell transplantation. This breakthrough addresses concerns about cell survival after implantation while delivering similar therapeutic effects.
Cell-free treatments like exosome therapy look especially promising. These treatments work well against osteoporosis without side effects. They might finally deliver the long-term bone health improvements that traditional drugs failed to achieve.
Research and clinical results show that stem cell therapy could revolutionize osteoporosis treatment. Traditional medications only slow down bone loss, but stem cell treatments actively help regenerate tissue through several pathways. Regencord’s method stands out because it tackles both excessive bone breakdown and reduced bone formation simultaneously.
Success stories from patients and research data prove that stem cell therapy works. Patients show better bone density measurements, and their quality of life improves substantially. These outcomes give hope to patients who haven’t seen results with standard treatments.
Regenerative medicine paints a bright future for osteoporosis treatment. Cell-free methods that use stem cell-derived vesicles show amazing results, and researchers continue to improve treatment protocols. Stem cell therapy helps trigger the body’s natural healing processes and provides a long-term solution for bone health. This represents a fundamental change from traditional treatment approaches.
We focus on knee treatment using stem cell therapy, focusing on three main processes:
Stem cells are unique cells with the ability to develop into various cell types and repair damaged tissues. They are used in regenerative medicine, including treatments for cancer, neurodegenerative diseases, and injuries. Sources include bone marrow, cord blood, and embryos.
+1 888-540-4101


