Multiple System Atrophy (MSA) affects just 1.90-4.90 people per 100,000 each year. This makes stem cell treatment a significant area of medical advancement for this neurodegenerative disease. Patients typically live 7-9 years after MSAvative treatments now give them new hope.
Traditional treatments only help with symptoms, but recent breakthroughs in stem cell therapy reveal remarkable possibilities. Specialized facilities like Regencord in Pereira, Colombia, have shown great success with human umbilical cord blood mononuclear cells. They have treated over 30 cases successfully through their advanced lateral atlantooccipital space puncture technique. Patient mobility and overall quality of life improved significantly, as proven by documented outcomes.


“Multiple system atrophy is a rare condition. Experts estimate an average of 0.6 to 0.7 new cases per 100,000 people yearly. The estimated number of total cases is between 3.4 and 4.9 per 100,000 people.” — Cleveland Clinic Medical Staff, Medical experts at Cleveland Clinic.
Multiple System Atrophy (MSA) takes a heavy toll on people’s lives. This neurological condition affects both quality of life and life expectancy. Let’s look at why patients look beyond standard care for advanced treatment options.
Multiple System Atrophy is a rare brain disorder that damages the nervous system. The brain’s vital areas break down over time, disrupting motor functions and automatic body processes. People used to know MSA by other names, such as Shy-Drager syndrome, olivopontocerebellar atrophy, and striatonigral degeneration. The condition usually starts between ages 50 and 60, though it can affect anyone over 30.
MSA is quite rare. Only 2 to 5 people in every 100,000 have this condition. The disease damages three key brain areas: the basal ganglia controls movement and learning, the brainstem manages breathing and heart rate, and the cerebellum coordinates balance and movement.
Inside the brain, MSA causes a protein called alpha-synuclein to build up abnormally in brain cells, particularly in oligodendrocytes. This leads to ongoing cell damage and neuronal degeneration. Doctors split MSA into two main types based on the main symptoms: MSA-P (multiple system atrophy parkinsonian type) and MSA-C (cerebellar type).
MSA symptoms get worse as time goes on. Each type shows different signs, but both affect the body's automatic functions, leading to autonomic dysfunction.
MSA-P patients deal with symptoms like Parkinson's disease, exhibiting Parkinsonism. Their muscles become stiff, balance gets poor, movements slow down, and some develop tremors. MSA-C patients face different challenges. They struggle with coordination, walking becomes difficult, they fall often, and their speech turns slurry, indicating cerebellar ataxia.
Both types share several serious nervous system problems:
MSA progresses faster than Parkinson's disease. Most patients need walking aids within a few years. People live about 7.5 to 9.8 years after symptoms start, though each case differs. The disease hits people's quality of life hard. Most patients say mobility becomes their biggest challenge.
Later stages bring more severe motor symptoms that affect daily life. Swallowing becomes harder, which might lead to pneumonia. On top of that, many patients develop depression and anxiety, making life even tougher.
We don't have a cure for MSA yet, and current treatments can't slow down or stop the disease. Doctors focus on symptomatic management to keep patients comfortable and independent for as long as possible.
Available medications include:
These treatments become less helpful as the disease progresses. Standard care doesn't meet all patient needs, so many look for other options.
Patients need help from many specialists. Neurologists, physical therapists, and speech pathologists work together to provide complete care. This team approach helps with symptoms but can't change how the disease develops.
The limits of current treatments push many families to explore new options. They look into emerging treatments like stem cell therapy, hoping to find something that might change the disease's course instead of just easing symptoms.
Stem cell therapy shows great promise in treating progressive neurodegeneration in multiple system atrophy. Traditional treatments only provide symptom relief, but cellular therapies might slow down disease progression and lead to better patient outcomes.
Stem cell treatment for multiple system atrophy works through several important mechanisms. We found that stem cells protect neurons by releasing neurotrophic factors like brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF). These factors help neurons survive and reduce cell death. They create better conditions for existing brain cells and might slow down the neurodegenerative process.
Stem cells also regulate the immune system effectively through immunomodulation. They reduce pro-inflammatory immune cells and boost anti-inflammatory cytokines like interleukin-10 and transforming growth factor-beta. This immune regulation helps a lot with MSA because inflammation makes the disease worse.
Stem cells help create new blood vessels by releasing vascular endothelial growth factor (VEGF). Better blood flow brings more nutrients to damaged brain areas and supports healing and function, contributing to brain repair.
Research backs up these benefits. A randomized trial showed that MSA patients who received mesenchymal stem cells had much smaller increases in Unified MSA Rating Scale scores than the placebo group, which meant slower disease progression. PET scans showed more cerebral glucose metabolism in the cerebellum and frontal white matter of treated patients, while the control group's metabolism decreased in these areas.
Several types of stem cells could help treat MSA:
Autologous stem cells, derived from the patient's own body, look promising for neurological conditions. They work best when they come from the patient's own body, which reduces rejection risks.
The success of stem cell therapy depends on getting cells to the right place. Common methods include:
Doctors use intra-arterial infusion to send stem cells straight to brain tissues through cerebral arteries. This gets more cells to affected areas but might cause small ischemic lesions in some cases.
Intravenous delivery offers the safest and simplest option. Stem cells travel through the body after injection, and some find their way to damaged brain regions by following inflammatory signals. Clinical trials show this method works for MSA patients with few side effects.
An intrathecal injection puts stem cells directly into the cerebrospinal fluid around the brain and spinal cord through lumbar puncture. This lets cells spread throughout the central nervous system and reach multiple affected areas.
Scientists have improved delivery systems. They can use magnetic fields to guide cells with magnetic nanoparticles to specific brain regions. They also modify cell surfaces to help stem cells find damaged tissues more easily, which improves treatments.


“Regencord in Pereira, Colombia, specializes in advanced stem cell therapies, providing innovative solutions for patients seeking effective and sustainable relief from osteoarthritis symptoms.” — PlacidWay Medical Tourism, International medical tourism company.
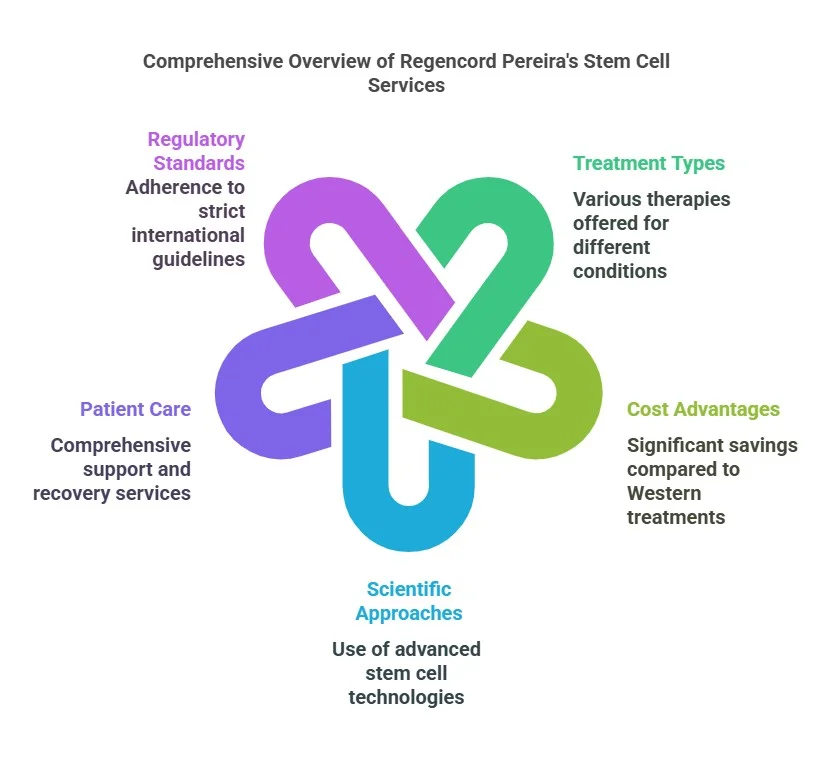
Regencord Colombia stands out as a premier destination for stem cell treatment for multiple system atrophy. The center’s detailed approach tackles MSA’s unique challenges through specialized care that goes beyond regular therapies.
Regencord Colombia has created targeted protocols specifically for neurological conditions, including MSA. Their method uses mesenchymal stem cells (MSCs) with remarkable regenerative, anti-inflammatory, and immune-regulatory properties. These protocols deliver stem cells through strategic methods—either intravenously or directly into the spinal fluid, depending on each patient’s condition.
Research shows that MSCs administered intrathecally for MSA patients were well-tolerated without serious adverse events. This treatment creates a marked rise in neurotrophic factors in spinal fluid that stays present for at least four weeks after administration. These factors create a more supportive environment that helps neuronal survival and potential repair.
Regencord's medical team brings unique experience to MSA treatment. Dr. Julieta Henao Bonilla leads the team as a medical geneticist with 30 years of experience in genome management and biotechnology. Dr. Carlos Alberto Isaza Mejia works with her as a physician pharmacologist, bringing three decades of research and teaching expertise.
The team combines over 60 years of experience in genetics, biotechnology, and pharmacology fields that directly relate to stem cell applications. Unlike centers that offer general care, Regencord's specialists have specific expertise in cellular therapy and regenerative medicine. This ensures patients get scientifically sound treatments based on solid research.
Regencord's laboratory meets the exceptional standards needed for advanced stem cell processing. The facility follows several ISO standards that ensure quality and safety:
This advanced facility lets them control each treatment step—from cell collection to final administration. Over the last decade, the center has treated more than 5,000 patients worldwide. It has strong protocols to maintain cell quality and viability.
Regencord's Stem Cell and Biotechnology Center maintains strict quality control throughout all processes, from biological sample collection through cellular concentrate release. Their steadfast dedication to international standards places them at the vanguard of regenerative medicine in Colombia, which has become a leading destination for advanced stem cell therapies.
The ground results of stem cell treatment for multiple system atrophy are clearly visible in patient outcomes at Regencord Colombia. Clinical results show real improvements in patients’ function and feelings.
The clinical data shows big improvements in mobility after stem cell treatments. The patient, who got autologous stem cells from his fat tissues, saw his symptoms slow down a lot. He went back to living an active life that he couldn’t manage before treatment. The improvements show up in the numbers, too. Patients who got mesenchymal stem cells did better on mobility tests. They scored higher on rotarod assessments (133.6 ± 7.29 seconds versus control groups) and grip strength tests (13.7 ± 1.18 seconds). Clinical trials showed that MSC-treated patients scored much higher on the unified MSA rating scale than control groups throughout a year-long study.
The changes go beyond just numbers and tests. The patient struggled with severe atopic dermatitis until his first stem cell treatment at Regencord immediately helped him. His inflammation went down quickly, and the complete therapy improved his condition by about 90%. MSA patients who got stem cell therapy could do daily tasks better and think more clearly even months later. Many patients who were stuck at home because of severe symptoms started getting out and living independently again.
Regencord's treatment benefits last. PET scans of treated MSA patients showed better glucose metabolism in the cerebellum and frontal white matter - key areas that MSA attacks. Control groups showed these areas getting worse. Patients in longer studies got more intrathecal MSC treatments every six months. This kept their disease from getting worse as fast as expected. The treatments worked less well in later stages but stayed safe with no serious side effects. Regencord keeps track of everyone's progress through scheduled check-ups to see how they're doing and adjust their treatment plans when needed.


Patients who start their stem cell treatment for multiple system atrophy at Regencord Colombia begin a well-laid-out therapeutic trip designed to maximize treatment results and ensure comfort and safety.
Regencord’s specialists conduct a detailed evaluation to start the treatment pathway. Their doctors review medical history, perform physical examinations, and run neurological tests to get a full picture of MSA symptoms. Advanced neuroimaging helps the medical team learn about neuronal damage and find specific affected brain regions that need targeting. This evaluation creates the foundation to determine treatment suitability and establish baseline measurements for tracking progress.
Stem cell treatment for Multiple System Atrophy stands as the most important breakthrough to help patients with this rare but devastating condition. Traditional therapies can only ease the symptoms, but Regencord Colombia has developed specialized protocols that show promising results. Their innovative approach uses mesenchymal stem cells and advanced delivery methods.
The treatment's effectiveness is shown in patient outcomes, with clear improvements in mobility and quality of life and slower disease progression. MSA patients receive treatment that meets international standards at state-of-the-art facilities. The expert medical teams provide complete follow-up care to ensure the best possible results.
Medical evidence proves stem cell therapy is a viable treatment option for MSA patients. Patient success stories, combined with Regencord's strict protocols and skilled specialists, bring new hope to people looking beyond traditional symptom management. These breakthroughs mark the most important progress in treating Multiple System Atrophy. Patients now have evidence-based options to manage this challenging condition better.
Recent MSA studies and new treatments for MSA in 2023 continue to show promise, with ongoing research into innovative approaches like immunomodulation and targeted brain repair techniques. As we gain more understanding of this complex neurodegenerative disease, the potential for more effective treatments grows, offering hope to those affected by MSA.
Stem cell therapy revolutionizes treatment options for osteopetrosis patients and provides hope beyond traditional treatments. Research shows the most important improvements happen in bone structure and blood formation, especially when patients start treatment early. The specialized protocols at Regencord’s Pereira facility have led to soaring wins, with the best results coming from patients who receive transplants before reaching 10 months.
Patients face several challenges, but quality of life improves substantially with proper post-transplant care and monitoring. They experience fewer fractures, move better, and enjoy improved health outcomes. Medical teams conduct regular follow-ups to ensure the best recovery and quickly address any complications.
Advanced stem cell therapies show great promise for treating osteopetrosis effectively. Success stories from children and adults prove these treatments work well regardless of age or condition severity. We have a long way to go, but we can build on this progress as medical science brings new hope to people affected by this challenging genetic disorder.
We focus on knee treatment using stem cell therapy, focusing on three main processes:
Stem cells are unique cells with the ability to develop into various cell types and repair damaged tissues. They are used in regenerative medicine, including treatments for cancer, neurodegenerative diseases, and injuries. Sources include bone marrow, cord blood, and embryos.
+1 888-540-4101


